Intravenous contrast-enhanced sonography in children and adolescents – a single center experience
Martin Stenzel
 Affiliation and address for correspondence
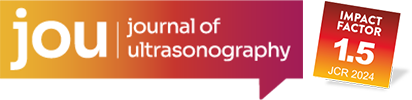
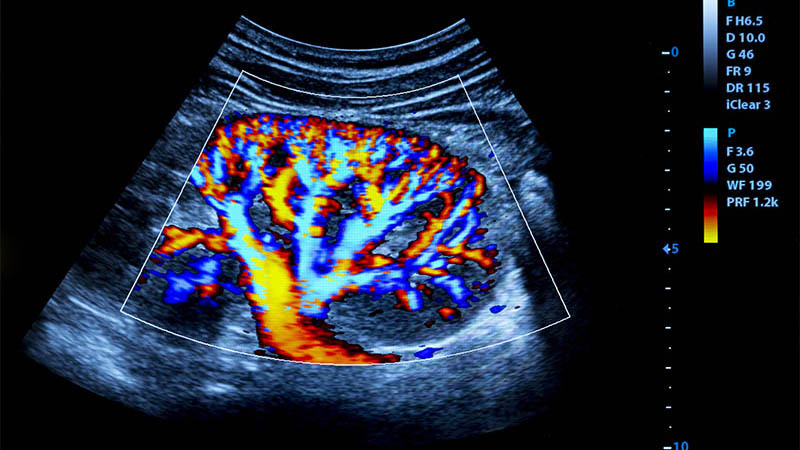
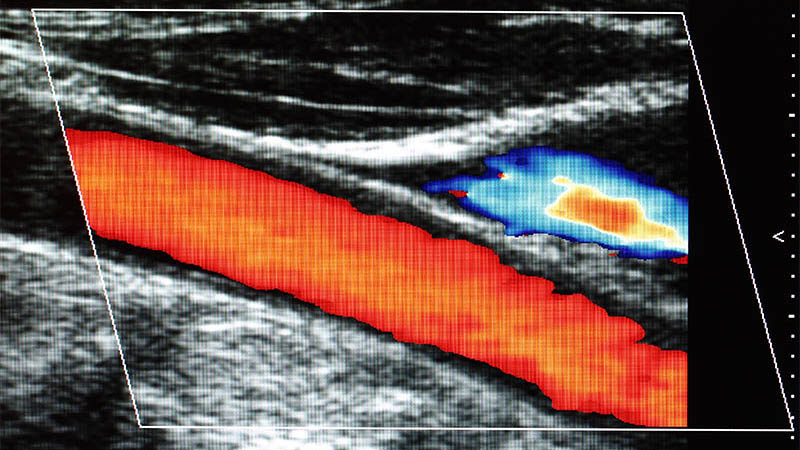
Affiliation and address for correspondenceCompared to adult patients, ultrasonography in children and adolescents is much more common, due to lack of ionizing radiation, and its wide availability. With the introduction of contrast-media for use in ultrasonography, one major drawback of the method could be overcome. In Europe, SonoVue® is the only widely available agent, which due to improved stability makes it possible to image normal and diseased tissue perfusion and vascularization with high accuracy. Inability to hold the breath and voluntary body movement of the patient is less of an obstacle compared to color Doppler techniques and makes the method very attractive for use in children, which, depending on age, may not be very cooperative. Use of intravenous contrast-medium in minors is currently very limited for several reasons: availability, lack of recommendation in national and international guidelines, and lack of official licensing. The article will touch medical indications, technique, safety considerations, and perspective of intravenous use of contrast-media in children and adolescents, including data from a 6-year period in 37 patients. Purpose: The purpose of the study was to collect data on ultrasonographic examinations, expanded by intravenous administration of the contrast agent SonoVue® in children and adolescents. Besides assessing diagnostic yield, data on adverse medication effects was collected. Materials and methods: The study includes contrast-enhanced ultrasound examinations in 37 children at a single institution. Indications for the examinations were tumor lesions, infections, traumatic organ injuries, and parenchymal organ ischemia. Parents of the patients and adolescent patients were informed about the off-label use of the contrast agent. Thirty-nine examinations were performed, the average age of the patient was 11.1 years (range 1 7/12 to 17 11/12 years). Results: All of the examinations yielded additional diagnostic value, always expanding results from B mode and color coded sonography. Overall, most examinations were done to assess the liver (n=16), followed by the kidney in 10 cases. The different etiologies were encountered in the following order: tumor (n=22), infection (n=9), trauma (n=5), ischemia (n=4). Most examinations were performed to evaluate a hepatic lesion (n=12). There was one incident recorded that fit the criteria of a possible adverse effect. In an 8-year-old girl nausea was noted, that started 15 minutes after the end of the examination and resolved spontaneously. In none of the patients medical treatment for adverse effects was necessary. Conclusion: Ultrasonography in children, enhanced by intravenous use of contrast medium is feasible and allows for further evaluating cystic and solid tumors, and organ perfusion. Given that proper medical equipment and correct ultrasound machine settings are used, it is a robust method without diagnostic failures. In this small-sized case series there were no severe adverse effects, however, off-label use in children needs to be addressed.