The usefulness of ultrasound in the diagnostics of Sjögren’s syndrome
Fadhil Saied1, Monika Włodkowska‑Korytkowska1,2, Maria Maślińska3, Brygida Kwiatkowska3, Wojciech Kunisz1, Patrycja Smorawińska1, Iwona Sudoł‑Szopińska1,2
 Affiliation and address for correspondence
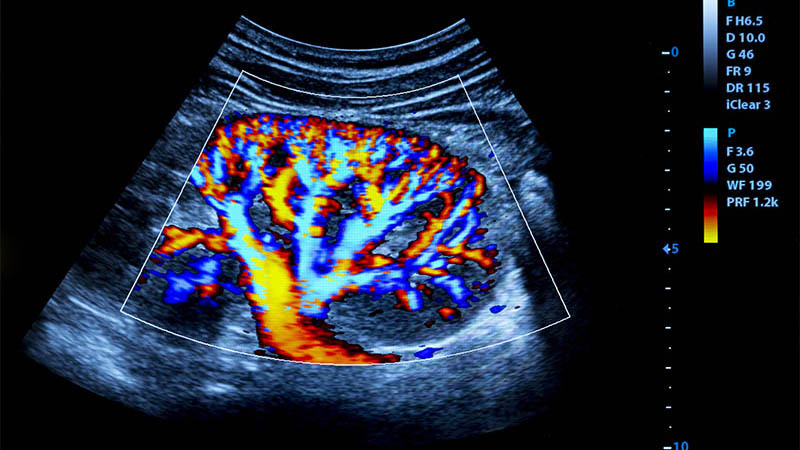
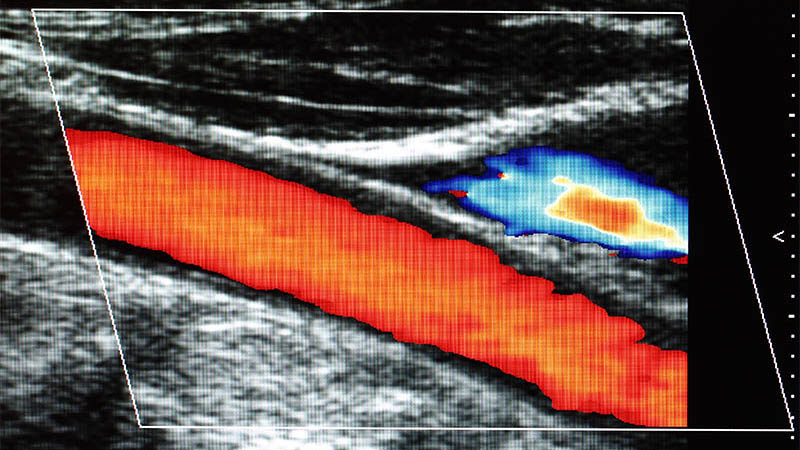
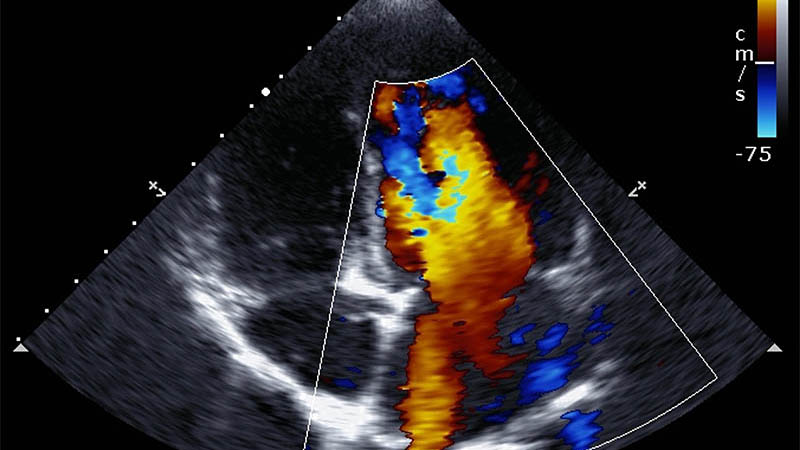
Affiliation and address for correspondenceSjögren’s syndrome is an autoimmune exocrinopathy which manifests itself with dryness of the eyes and the oral cavity. These symptoms comprise a so-called sicca syndrome (xerostomia and xerophthalmia). Two forms of this disease may be distinguished: primary Sjögren’s syndrome which affects salivary glands and secondary Sjögren’s syndrome with other autoimmune diseases present such as rheumatoid arthritis, systemic lupus erythematosus or systemic scleroderma. The diagnosis is based on the classification criteria established in 2002 by a group of American and European scientists (American-European Consensus Group), which involve the interview and physical examination as well as serological, histopathological and radiological tests. Most of these examinations show some limitations such as invasiveness, expensiveness or limited accessibility. The latest research suggests that ultrasound examination may appear promising in the diagnostics of the main salivary glands: submandibular and parotid glands. It is an accessible and relatively cheap examination with high sensitivity and specificity values which are comparable to those obtained via conventional means used in the diagnostics of this disease, i.e. biopsy of the minor salivary glands, sialography and scintigraphy, as well as superior to those obtained in sialometry and Schirmer’s test. Additionally, ultrasonography correlates with the results of magnetic resonance imaging. Therefore, a number of authors claim that US examination should be included in the classification criteria of Sjögren’s syndrome. The aim of this article is to present the diagnostic capacity of the US examination in Sjögren’s syndrome using the current ultrasound classification systems based on the grey-scale, Doppler and contrast-enhanced examinations. The latest research confirms that the most valuable diagnostic criterion in Sjögren’s syndrome is the heterogeneity of the glandular parenchyma. The outcome of the examination greatly depends on the examiner’s experience.