Endosonography and magnetic resonance imaging in the diagnosis of high anal fistulae – a comparison
 Affiliation and address for correspondence
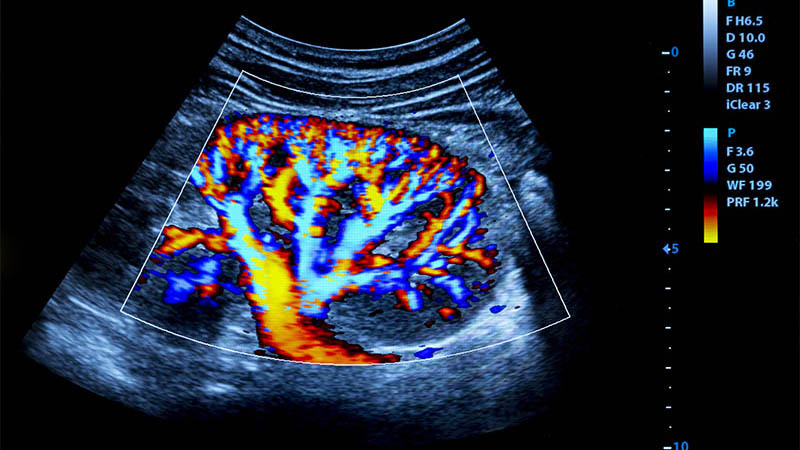
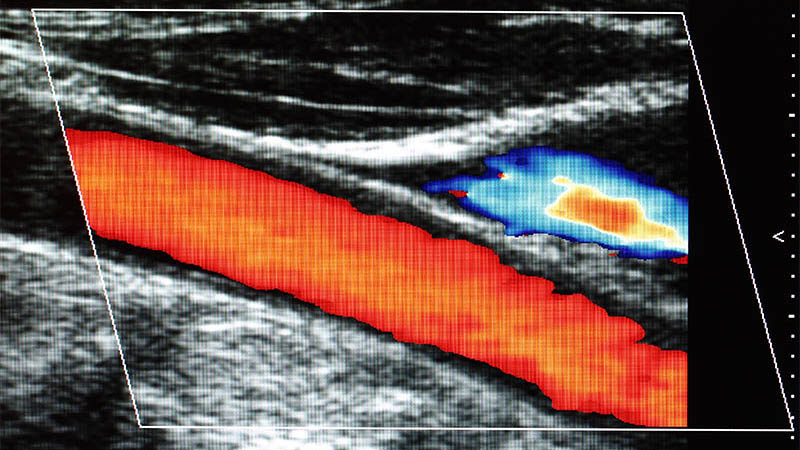
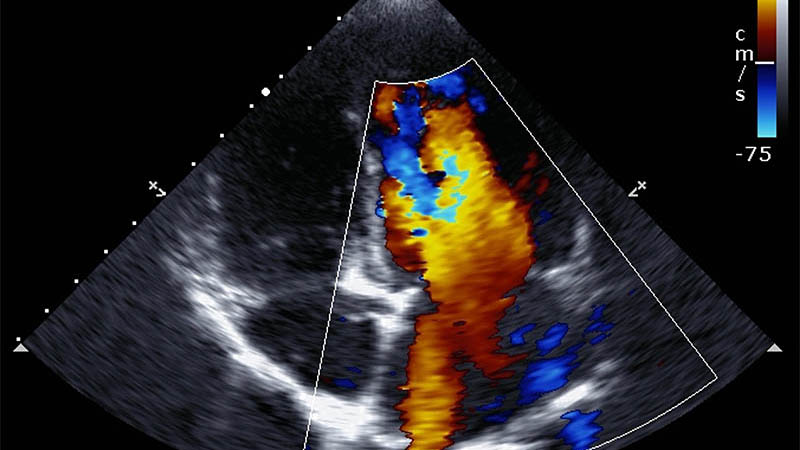
Affiliation and address for correspondenceAnal fistula is a benign inflammatory disease with unclear etiology which develops in approximately 10 in 100 000 adult patients. Surgical treatment of fistulae is associated with a risk of damaging anal sphincters. This usually happens in treating high fistulae, branched fistulae, and anterior ones in females. In preoperative diagnosis of anal fistulae, endosonography and magnetic resonance imaging play a significant role in planning the surgical technique. The majority of fistulae are diagnosed in endosonography, but magnetic resonance is performed when the presence of high fistulae, particularly branched ones, and recurrent is suspected. The aim of this paper was to compare the roles of the two examinations in preoperative assessment of high anal fistulae. Material and methods: The results of endosonographic and magnetic resonance examinations performed in 2011–2012 in 14 patients (4 women and 10 men) with high anal fistulae diagnosed intraoperatively were subject to a retrospective analysis. The patients were aged from 23 to 66 (mean 47). The endosonographic examinations were performed with the use of a BK Medical Pro Focus system with endorectal 3D transducers with the frequency of 16 MHz. The magnetic resonance scans were performed using a Siemens Avanto 1.5 T scanner with a surface coil in T1, T1FS, FLAIR, T2 sequences and in T1 following contrast medium administration. The sensitivity and specificity of endosonography and magnetic resonance imaging were analyzed. A surgical treatment served as a method for verification. The agreement of each method with the surgery and the agreement of endosonography and magnetic resonance imaging were compared in terms of the assessment of the fistula type, localization of its internal opening and branches. The agreement level was determined based on the percentage of consistent assessments and Cohen’s coefficient of agreement, κ. The integrity of the anal sphincters was assessed in each case. Results: In determining the fistula type, magnetic resonance imaging agreed with intraoperative assessment in 79% of cases, and endosonography in 64% of cases. Endosonography agreed with magnetic resonance in 57% of cases. In the assessment of internal opening, the agreement between endosonography and intraoperative assessment was 65%, between magnetic resonance and intraoperative assessment – 41% and between endosonography and magnetic resonance – 53%. In the assessment of fistula branches, endosonography agreed with intraoperative assessment in 67% of cases, magnetic resonance in 87% of cases, and the agreement between the two methods tested was 67%. Conclusions: Magnetic resonance is a more accurate method than endosonography in determining the type of high fistulae and the presence of branches. In assessing the internal opening, endosonography proved more accurate. The agreement between the two methods ranges from 53–67%; the highest level of agreement was noted for the assessment of branching.