Editorial Comment on: Andrzej Smereczyński, Teresa Starzyńska, Katarzyna Kołaczyk and Józef Kładny Role of sonography in assessing complications after laparoscopic cholecystectomy
Wiesław Tarnowski
 Affiliation and address for correspondence
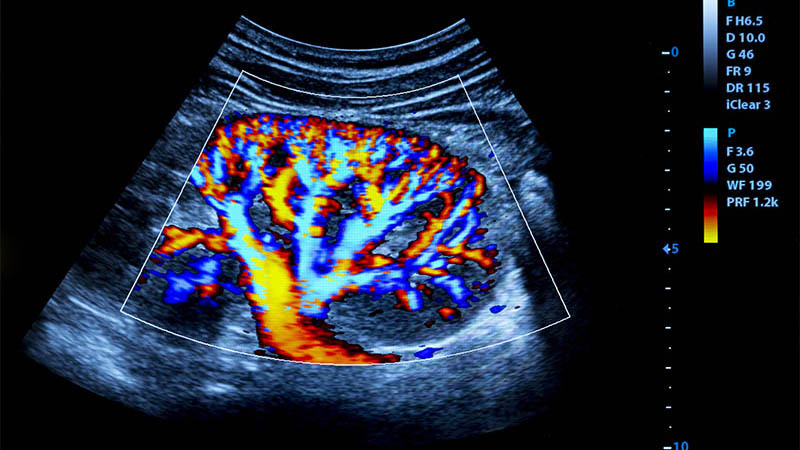
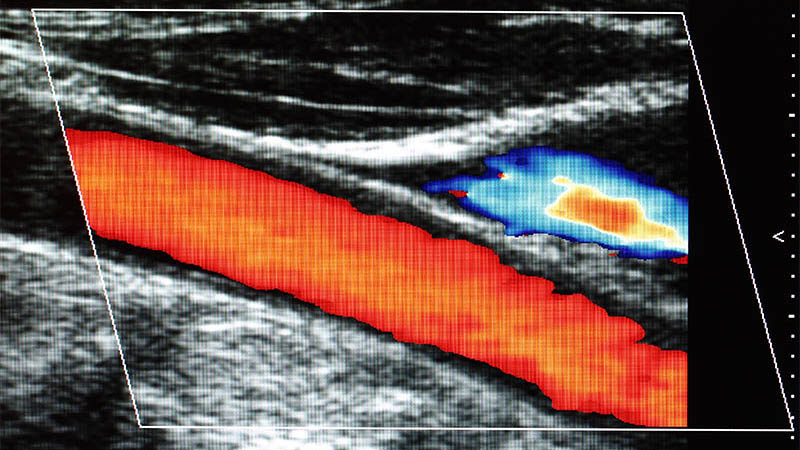
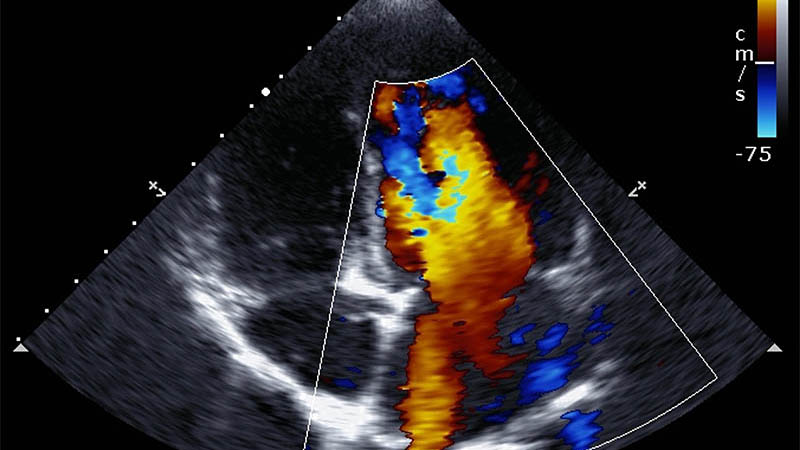
Affiliation and address for correspondenceLaparoscopic cholecystectomy (LC) was introduced to the arsenal of surgical techniques in 1987 and has become the gold standard in treating cholecystolithiasis. In spite of undoubted benefits for patients, it is not a complication- free procedure. The type of complications after a classical, i.e. “open” surgery and LC do not differ in a significant way. The difference lies in their prevalence. One of the most common complications is a fluid collection in the gallbladder bed under the liver. To prevent it from developing, a drain is usually placed under the liver. For many years, it was believed that such a practice is correct, but recent reports indicate that leaving the drain after a planned laparoscopic cholecystectomy may do more damage rather than be beneficial. Moreover, it may give a false impression of safety since we are convinced that we remain in control over the situation in case of, for instance, a hemorrhage (1) . In fact, when the postoperative bleeding to the peritoneal cavity is intense, a thin Redon drain, which usually remains inserted after the procedure, may become occluded by a thrombus. Decisions are made based on the patient’s clinical condition or imaging examinations (including sonography) which can reveal not only a fluid collection under the liver, but also free fluid in the peritoneal cavity.