Role of high-resolution ultrasonography in the evaluation of the tibial and median nerves in diabetic peripheral neuropathy
Tanu Ranjan, Shruti Chandak, Ankur Malhotra, Arjit Aggarwal, Jigar Haria, Deepak Singla
 Affiliation and address for correspondence
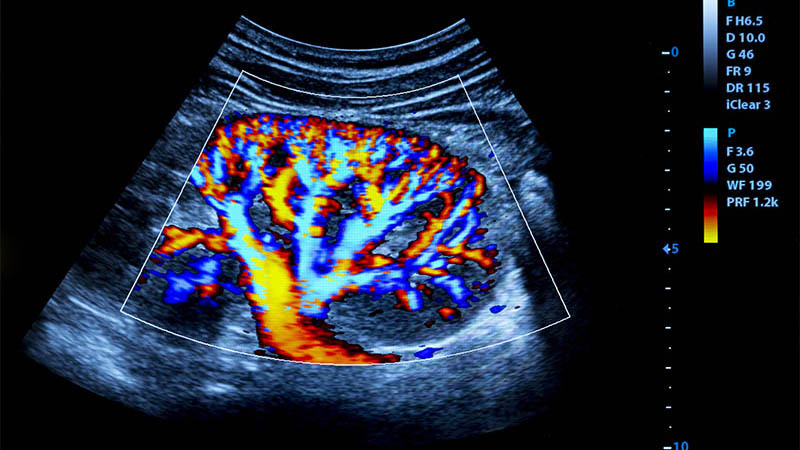
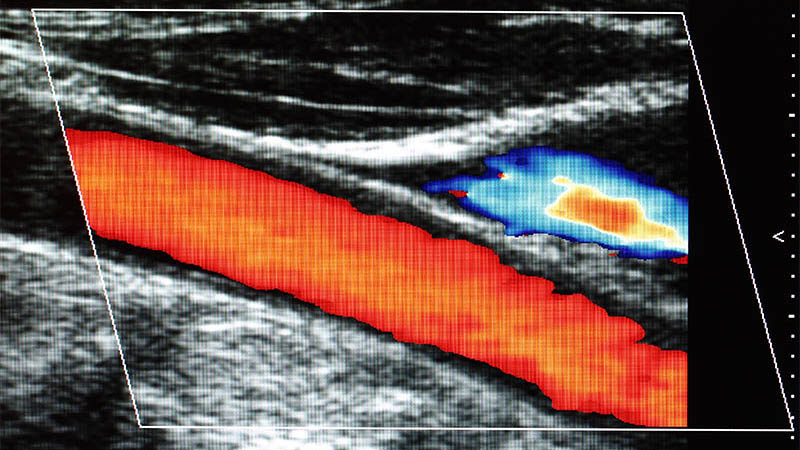
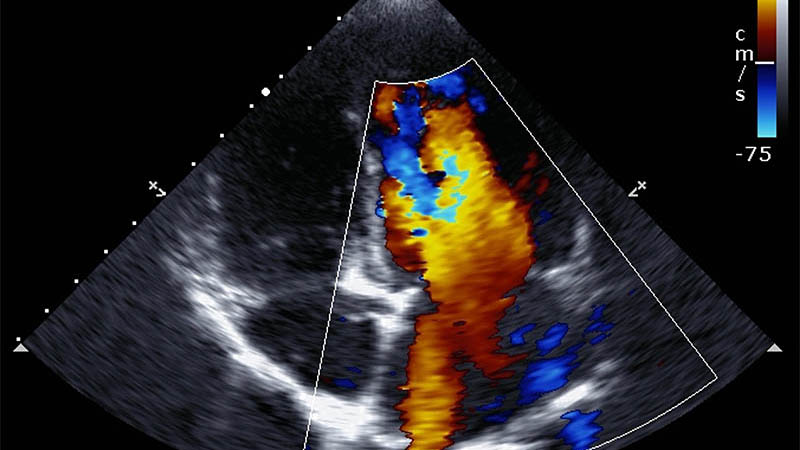
Affiliation and address for correspondenceAim: To evaluate and measure the mean cross-sectional area of the tibial and median nerves in patients with diabetic peripheral neuropathy, and to study the association between high-resolution ultrasonographic findings in diabetic peripheral neuropathy with the duration of illness, glycosylated haemoglobin values, random blood sugar levels, and aesthesiometry (using monofilament examination). Material and methods: A prospective observational study was conducted among 63 patients who were diagnosed with type 2 diabetes mellitus and underwent ultrasound and monofilament examinations. The cross-sectional area of the median nerve of the dominant hand and the tibial nerves was calculated on ultrasound examination. Results: The mean cross-sectional area of the median and tibial nerves was higher in patients with poor glycaemic control, with the mean cross-sectional area of the median nerve being 10.9, 12.8, 13.0, and 12.9 mm2 at various points in the leg in cases where the monofilament examination was negative, as compared to 7.30, 7.78, 7.91, 7.87 mm2 in patients with positive monofilament examination results. There was a significant positive correlation between the cross-sectional area of the tibial and median nerves and HbA1c, duration of diabetes, aesthesiometry, and random blood sugar levels. With an increase in HbA1c, duration of diabetes, and random blood sugar levels, there was a corresponding increase in the cross-sectional area of the nerves. These findings helped us to identify diabetic peripheral neuropathy. Conclusions: High-resolution ultrasonography along with aesthesiometry and HbA1c values can be an effective and easily available tool for detecting changes secondary to diabetic peripheral neuropathy. The method has a potential to replace or substitute nerve conduction tests in the near future.