Role of high-resolution ultrasound and magnetic resonance neurography in the evaluation of peripheral nerves in the upper extremity
Ali Serhal1, Steven Kyungho Lee1, Julia Michalek2, Muhamad Serhal1, Imran Muhammad Omar1
 Affiliation and address for correspondence
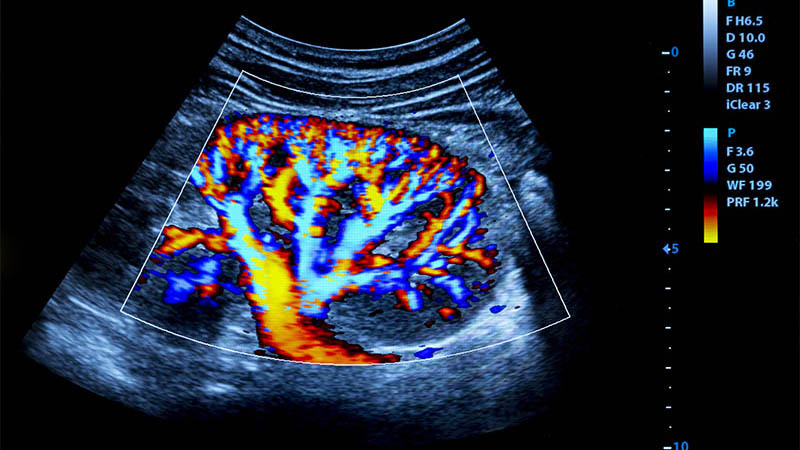
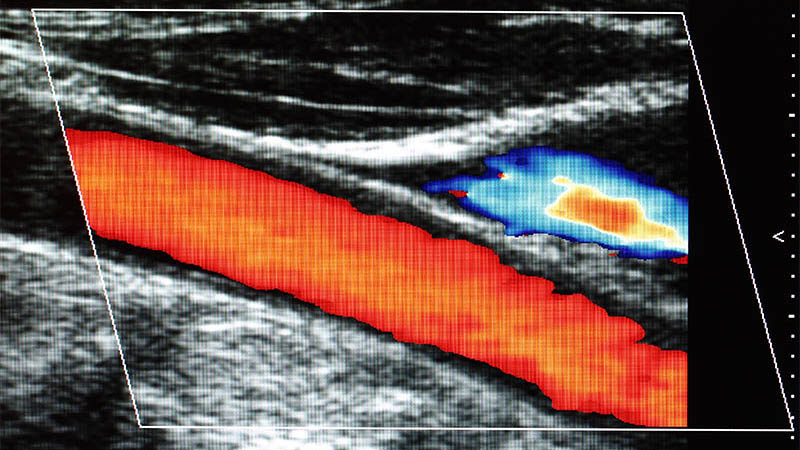
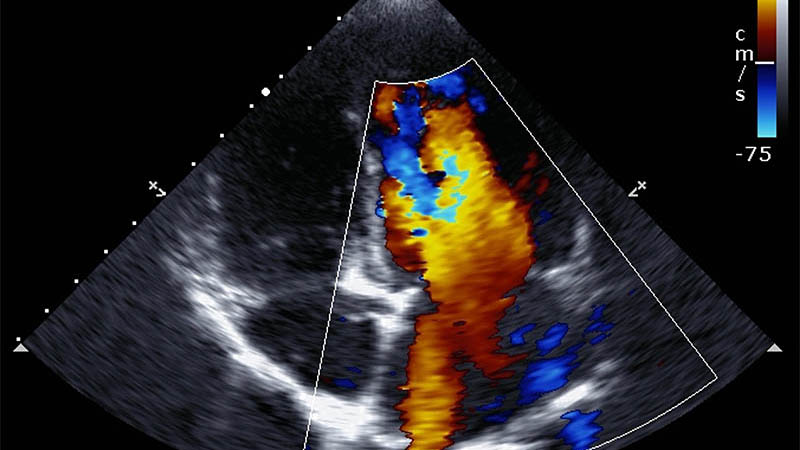
Affiliation and address for correspondenceUpper extremity entrapment neuropathies are common conditions in which peripheral nerves are prone to injury at specific anatomical locations, particularly superficial regions or within fibro-osseous tunnels, resulting in pain and potential disability. Although neuropathy is primarily diagnosed clinically by physical examination and electrophysiology, imaging evaluation with ultrasound and magnetic resonance neurography are valuable complementary non-invasive and accurate tools for evaluation and can help define the site and cause of nerve dysfunction which ultimately leads to precise and timely treatment. Ultrasound, which has higher spatial resolution, can quickly and comfortably characterize the peripheral nerves in real time and can evaluate for denervation related muscle atrophy. Magnetic resonance imaging on the other hand provides excellent contrast resolution between the nerves and adjacent tissues, also between pathologic and normal segments of peripheral nerves. It can also assess the degree of muscle denervation and atrophy. As a prerequisite for nerve imaging, radiologists and sonographers should have a thorough knowledge of anatomy of the peripheral nerves and their superficial and deep branches, including variant anatomy, and the motor and sensory territories innervated by each nerve. The purpose of this illustrative article is to review the common neuropathy and nerve entrapment syndromes in the upper extremities focusing on ultrasound and magnetic resonance neurography imaging.