Value of ultrasonography in the diagnosis of polycystic ovary syndrome – literature review
Michał Bachanek, Nebil Abdalla, Krzysztof Cendrowski, Włodzimierz Sawicki
 Affiliation and address for correspondence
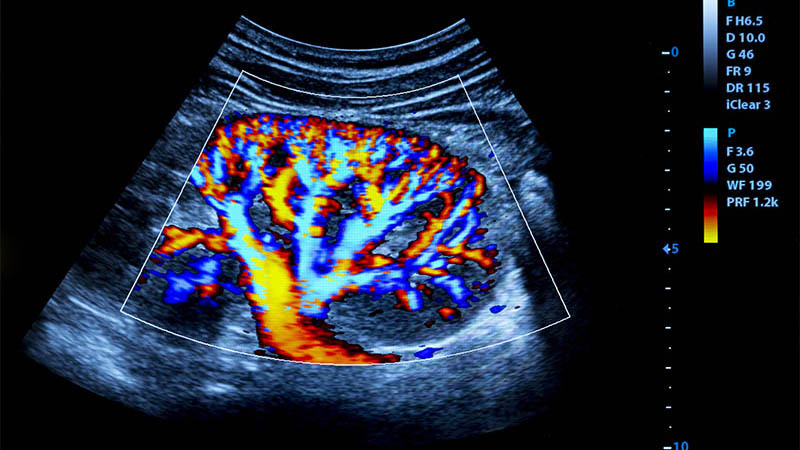
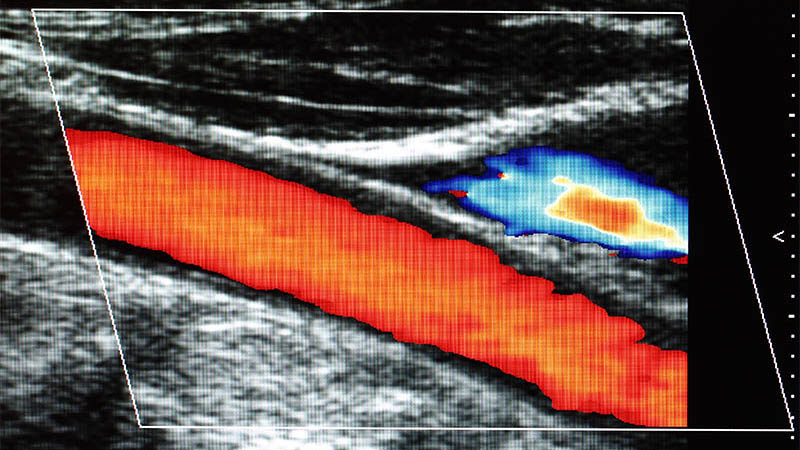
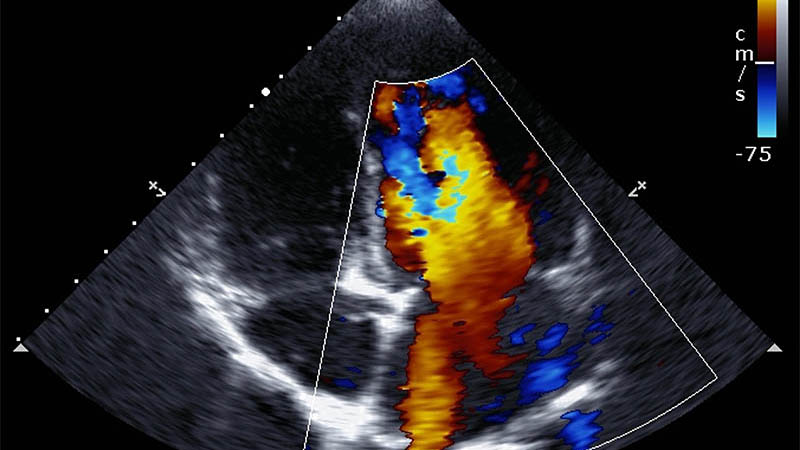
Affiliation and address for correspondencePolycystic ovary syndrome is a multi-factorial disease. Its etiopathogenesis has not been elucidated in detail. It is the most common endocrine disorder in women of child-bearing age. This disease entity is primarily characterized by disrupted ovulation and hyperandrogenism, but the clinical picture can be diversified and symptom intensity can vary. Currently, the sonographic assessment of ovaries is one of the obligatory criteria for the diagnosis of PCOS according to the Rotterdam consensus (2003) and Androgen Excess & PCOS Society (2006). This criterion is determined by the presence of ≥12 follicles within the ovary with a diameter of 2–9 mm and/or ovarian volume ≥10 cm3. Such an ultrasound image in one gonad only is sufficient to define polycystic ovaries. The coexistence of polycystic ovaries with polycystic ovary syndrome is confirmed in over 90% of cases irrespective of ethnic factors or race. However, because of the commonness of ultrasound features of polycystic ovaries in healthy women, the inclusion of this sign to the diagnostic criteria of polycystic ovary syndrome is still questioned. The development of new technologies has an undoubted influence on the percentage of diagnosed polycystic ovaries. This process has caused an increase in the percentage of polycystic ovary diagnoses since the Rotterdam criteria were published. It is therefore needed to prepare new commonly accepted diagnostic norms concerning the number of ovarian follicles and the standardization of the technique in which they are counted. The assessment of anti-Müllerian hormone levels as an equivalent of ultrasound features of polycystic ovaries is a promising method. However, analytic methods have to be standardized in order to establish commonly accepted diagnostic norms.